Jeremy Smith, MD is a highly regarded surgeon with a remarkable passion, unwavering commitment, and exceptional expertise in the field of spinal deformity and reconstruction surgery. Dr. Smith has been a part of the Orange County community for several years, serving as Chief of Spine Surgery at Hoag Orthopaedic Institue, Orange County’s premier destination for orthopaedic surgery. His remarkable patient outcomes are a testament to his surgical proficiency and compassionate approach.
Spinal reconstruction surgery is used to correct significant deformities and stabilize the spine, using rods, pins, and fusion techniques. Reconstruction surgery is commonly used to treat conditions such as scoliosis, spondylolisthesis, kyphosis, and more.
Committed to advancing spinal deformity surgery, Dr. Smith has made a profound impact through his clinical and academic work in this field. He has actively engaged in research, shedding light on innovative approaches and advancements in spinal deformity surgery. His scholarly contributions have been recognized through numerous publications, further establishing his expertise and enhancing the knowledge base in his field.
Furthermore, Dr. Smith’s exceptional care extends to patients who have experienced previous surgical failures. With his expertise and comprehensive understanding of complex spinal deformities, he compassionately approaches each case, tailoring treatment plans to address the unique needs and challenges of these individuals. Contact us today to schedule an appointment to see how Dr. Smith can help you with your pain.
Treatment for scoliosis is based on an assessment of the curvature of the spine and the age of the patient. Depending on how mild or severe the condition may be, treatment for scoliosis may range from bracing (to slow the progression of the disease) to surgery. The most common surgical procedure is correction, stabilization, and fusion of the curve.

Spinal fusions are the surgical joining together of two or more vertebrae into one stable piece. This procedure may be done through the belly (anterior) or the back (posterior). Spinal fusions are done so that the pain resulting from separate vertebral movements (and the discs and nerves connected to them) may be eliminated. The regions of the back are: cervical (upper), thoracic (mid), and lumbar (lower). A posterior spinal fusion surgery addresses pain resulting from degenerative spine disorders.


Spinal fusions correct problems with bones in the spine. Posterior refers to the positioning of the surgery approach (the back), as opposed to an anterior approach (the front). Fusion surgeries have the advantage of being done from any number of angles. Surgeons can achieve a minimally invasive surgical procedure by being purposeful with their initial approach – because there is less cutting of the tissue being done in order to reach the spine. This decision making allows for patients to have an easier time with their recovery and less or smaller incisions. Once the spine is reached during the procedure, multiple vertebrae are then fused together.
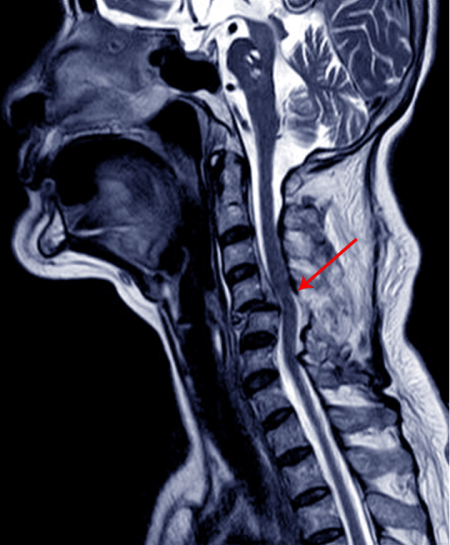
In order to stabilize the neck, two or more of the cervical vertebrae in the spine are fused together. Fractures or abnormal curvatures in the spine may also be treated with spinal fusions.
Usually, a surgeon will approach this procedure through a small incision in the front of the neck.
In order to stabilize the spine, two or more of the thoracic vertebrae are bonded, or “fused” together. Spinal stenosis may be treated with a spinal fusion. This procedure will also restore strength to the middle back portion of the spine.
The lumbar (lower back) region of the spine is most prone to spine fusion, as opposed to other regions of the spine, such as the cervical (neck) and the thoracic (mid-back) regions. Spinal fusion is usually recommended for neurological problems or for patients experiencing severe pain who have experienced little relief from more conservative treatments.


A corpectomy is a surgical procedure where the front part of the vertebrae, the vertebral body, is removed, but the bone that surrounds and protects the spinal cord is preserved. It is often accompanied by a discectomy, the surgical removal of an intervertebral disc. A thoracic corpectomy is performed in order to stimulate new bone growth between the upper and lower vertebrae. A surgeon will insert a structural cage into the open space between the vertebrae in order to encourage this.

The spine is made up of many small bones called vertebrae, and together, these vertebrae form the spinal column, which protects and houses the spinal cord. Any injury along the spine that occurs from the neck to the lower back can cause trauma – changes in our strength, our ability to experience sensation, and other body functions. Although spine trauma is often the result of a sudden impact or accident, there are also other factors that can increase the likelihood of an injury to the spine.
When a patient has continual problems from an earlier spine surgery, revision surgery may be necessary. This surgery addresses structural problems in the spine. Dr. Jeremy Smith is often sought out for this procedure, as he gives patients a second chance at a positive outcome. A patient still experiencing chronic pain, even after their initial spine surgery, may be experiencing unforeseen complications and must have the issue corrected. Revision surgery may be necessary for relief if painful scar tissue has formed around the spinal structures, for example. Patients need not lose hope – even if a revision may take multiple surgeries, Dr. Jeremy Smith is committed to follow-up x-rays and open communications the whole way through, until the spine’s structural damage is addressed appropriately and/or resolved. Many doctors refer patients to pain management professionals instead of seeking out solutions based on the source of the condition, but Dr. Jeremy Smith wants permanent working results for his patients. He believes that hope is worth pursuing for every patient.



Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur. Excepteur sint occaecat cupidatat non proident, sunt in culpaest laborum.
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.


There are both surgical and non-surgical options available for treating spinal infections. If there is no evidence of neurological deficits in a patient due to the infection, some non-surgical options may include long-term intravenous antifungal or antibiotic therapy for 6 to 8 weeks. Otherwise, surgery may be necessary in order to treat spinal infection when there is notable bone involvement, sepsis, failure of needle biopsy or a clear neurological deficit in the patient.