Cervical spine disorders target the vertebrae in the neck, and discs between each vertebrae and/or joints, muscles, and ligaments. These structures in the spine may degenerate over time, or quickly become less viable due to injury. Coordination may be affected by certain cervical spine conditions, and pain and numbness are also common symptoms.
Cervical stenosis is most common in adults over 50 years of age, and occurs when the spinal canal begins to narrow. This causes pressure to be put on the spinal cord, and surrounding nerves traveling through the spine. This “wear and tear” can then cause pain via pinching of the nerves, or, radiculopathy.

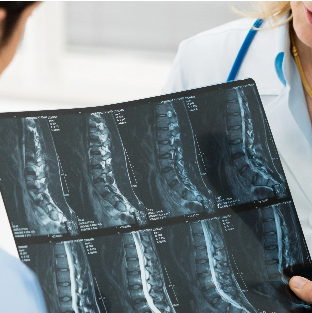
First, your doctor will make a diagnosis based on your medical history, a neurological exam, and the information collected from a series of diagnostic tests such as a X-rays, CT scans, MRI scans, or myelography (a radiographic exam used to detect pathology of the spinal cord). If cervical stenosis is found, it may be treated with a conservative approach, such as physical therapy, medications, steroid injections or acupuncture. Sometimes, in chronic condition or severe cases, these conservative measures are not adequate and cervical stenosis may require surgery to relieve symptoms.

Between the bones of the spine are small rubbery structures that allow for padding between the bone and the nerves called “discs”. When one of these discs “slip”, bulge, or rupture, a fragment of the disc can be pushed directly into the spinal canal. Slippage such as this can cause tremendous pain in the neck, back and arm. This is a common cervical condition and can be treated with minimally invasive surgery options.
During a physical examination, the doctor will analyze the neck’s movement in order to identify the source of the pain and any related injured tissue. Further testing such as an MRI and/or CT scan, a myelogram, X-rays, a nerve conduction velocity (NCV) or electromyography (EMG) may also aid in providing an accurate diagnosis of this condition. There are a variety of treatment options for this condition, both conservative and surgical. Conservative options include: adequate rest, ice/heat compression, physical therapy, massaging the neck, strengthening exercises, medications, steroid injections and a number of holistic therapies such as acupuncture, acupressure and even nutritional supplements. For patients who are not responding to these treatments, sometimes in part due to age, other medical conditions, or previous injuries, various technological advancements in surgery are available. Some techniques may include: anterior cervical discectomy and fusion (ACDF), artificial disc replacement and posterior cervical discectomy – which can now be performed through minimally invasive techniques,have a diminished recovery time, and improved success rate.

Pseudarthrosis occurs when a previous fusion surgery does not heal properly. New bone formation may not properly occur for a number of reasons. This can cause pain in the neck/spine, extremity pain, sensory changes, and in some cases, recurrence of pain that was initially resolved after the index surgery. There are risk factors associated with developing a pseudoarthrosis, some of which can be mitigated by the patient before surgery even occurs. The symptoms of pseudarthrosis can be vague, and imaging studies are important to properly assess a patient for this condition.


Pseudoarthrosis is ideally prevented, rather than treated. Prevention occurs through reducing risk factors inside the patient’s control – these are reviewed on a case-by-case basis as they are unique for each individual. In some cases, bone growth stimulators can be used immediately after surgery to encourage new bone growth. If pseudoarthrosis does occur, and is causing neurologic compromise/loss of function, it is typically addressed through a revision spinal surgery.

One of the most common causes of radiating arm and neck pain is cervical degenerative disc disease. This condition occurs with normal “wear and tear” of the cushioning discs in the cervical spine. Normal wear and tear could result from daily activities, sports injuries or even a simple “drying out of the disc”. While degenerative disc disease can start as a nagging pain and eventually become debilitating for a patient.
A physical and neurological exam, strength and sensitivity testing, and diagnostic imaging such as X-rays – which reveal collapsed disc space and the alignment of the spine – allow for a clear diagnosis of this condition. An initial non-surgical approach to this condition may include: medications, spinal injections, physiotherapy and acupuncture; while a minimally invasive surgical approach may be necessary for patients suffering from spinal instability or neurological dysfunction.

Cervical radiculopathy is a change in neurological function that results when a nerve root in the cervical spine (neck) becomes inflamed or damaged. When a nerve gets pinched or irritated in the neck, it can cause numbness, weakness or radiating pain into the arm or head. Cervical radiculopathy is very common and the condition most often improves on its own.


Your doctor may order an X-ray, MRI or CT scans, electromyography and nerve conduction studies after completing a physical exam in order to diagnose this condition. While medication, physical therapy, and pain-blocking injections are a conservative approach to treating this condition, the most common surgical treatment for cervical radiculopathy is a nerve root decompression. This involves removing the disc and fusing vertebrae above and below with a titanium plate. Herniated discs may also be replaced with artificial discs – these are used in place of a bone fusion to preserve the movement and flexibility of the neck. Another surgical option for this condition is a decompressive laminectomy and fusion. During this procedure, a portion of the bone (or lamina) that is forcing pressure onto the nerve, and thus causing pain, is removed.