If you have noticed that your back feels stiffer than it used to, or that long walks, yardwork, or even sitting too long now comes with a “price,” you are not alone. After 50, the spine naturally changes in ways that can affect flexibility, shock absorption, posture, and even how your nerves tolerate everyday movement. Some of these shifts are simply part of aging. Others are early signs of conditions that respond best when addressed sooner rather than later.
As a fellowship trained orthopaedic spine surgeon, Dr. Jeremy Smith helps patients understand what is normal, what is not, and what you can do to protect your mobility for the long run. The goal is not perfection. It is staying active, independent, and confident in your body as the years add up.
How the Spine Changes With Age
Think of your spine as a column built for motion and support. Over time, the structures that allow you to bend, twist, and absorb impact start to lose some of their “spring.” Around age 50 and beyond, these are the most common changes:
- Spinal discs gradually lose hydration and height. Discs act like cushions between the vertebrae, and they naturally dry out with age. Less hydration means less shock absorption. Reduced height can also change the spacing where nerves travel.
- Vertebrae may shift or compress as disc space narrows. When the disc loses height, the mechanics of the spine change. This can contribute to alignment issues and make certain segments work harder than they used to.
- Spinal joints develop wear and tear. The facet joints in the back of the spine guide motion. Like knees or hips, they can develop arthritis. That can lead to stiffness, inflammation, and pain with certain positions or movements.
- Ligaments can thicken and lose elasticity. Ligaments are meant to be supportive but flexible. With age, they can become less elastic and sometimes thicken, which may reduce space around nerves.
Muscles supporting the spine may weaken. Core and back muscles play a major role in posture and stability. If these muscles weaken, you may notice changes in alignment, endurance, or balance.
None of this means you are destined for severe pain. But it does explain why a spine that tolerated decades of work, sports, or daily wear may start to “talk back” after 50.
Common Spine Conditions in Adults Over 50
Many people assume back or neck pain is just part of aging. The truth is that common age related spine conditions have recognizable patterns, and many have effective treatment options.
Degenerative Disc Disease (DDD)
Despite the name, DDD is not a disease in the traditional sense. It is a term used to describe disc aging and breakdown. As discs thin and become less flexible, some people develop chronic neck or back pain, especially with sitting, bending, or lifting.
Spinal Stenosis
Stenosis means narrowing. In the spine, it often refers to narrowing of the spinal canal or the openings where nerves exit. This can cause leg pain, numbness, or heaviness with walking, sometimes relieved by sitting or bending forward. Many people describe it as their “legs giving out” or feeling like they cannot walk as far as they used to.
Facet Joint Arthritis
Facet arthritis can cause localized back pain and stiffness, often worse in the morning or after being still. It can also flare with standing and extension movements, like arching the back.
Spondylolisthesis
This occurs when one vertebra slips forward over another. In adults over 50, it is commonly related to degeneration rather than trauma. Symptoms range from back pain to nerve related symptoms, depending on whether nerves are being irritated.
Osteoporosis Related Fractures
As bones weaken, compression fractures can occur in the spine, sometimes after a fall, sometimes after a minor twist or lift. These fractures can cause sudden pain, height loss, and posture changes.
Recognizing Symptoms of Age-Related Spine Changes
Not every ache needs a specialist visit, but certain symptoms are worth paying attention to, especially if they are new, persistent, or worsening.
Common symptoms after 50 include:
- Stiffness or reduced range of motion in the neck or back
- Chronic lower back pain that lingers for weeks
- Radiating arm or leg pain, sometimes described as burning or electric
- Numbness or tingling in the hands, feet, arms, or legs
- Difficulty standing or walking for long periods
- Noticeable height loss or changes in posture, including a more stooped stance
A helpful way to think about symptoms is to separate “mechanical pain” from “nerve pain.” Mechanical pain is often localized and tied to movement or posture. Nerve pain tends to travel, tingle, or cause weakness. Both matter, but nerve symptoms deserve earlier evaluation.
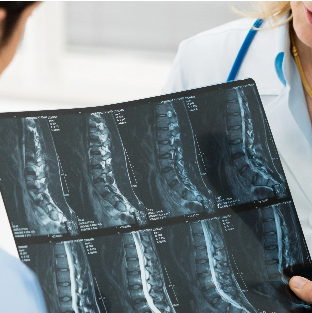
How Age-Related Spine Issues Are Diagnosed
Good spine care starts with an accurate diagnosis. Many conditions share overlapping symptoms, so guessing can lead to frustration and delayed relief. A thorough evaluation often includes:
- A physical exam to assess strength, flexibility, reflexes, gait, and neurological function. This helps identify whether a nerve is involved and which level may be the source.
- X rays to evaluate alignment, disc space narrowing, bone spurs, and instability.
- MRI to assess discs, spinal cord, nerve roots, and other soft tissues. This is often the best tool for understanding stenosis and nerve compression.
- CT scans when more detailed bone imaging is needed, especially in complex anatomy or when surgical planning requires a clearer look at bony structures.
- Bone density testing for patients at risk of osteoporosis, particularly if there is a concern for fracture or if prevention needs to be part of the plan.
In many cases, imaging confirms what the exam already suggests. But just as important, it helps match treatment to the true pain generator instead of chasing incidental findings.
Treatment Options for the Aging Spine
Most age related spine problems improve with non surgical care. When symptoms persist or neurological issues develop, surgical options may be appropriate. The best plans are individualized, because two people with the same MRI can have very different goals, activity levels, and health considerations.
Non Surgical Care
- Physical therapy is often the foundation. The right program focuses on core strength, hip mobility, posture, and movement patterns that protect the spine during daily life.
- Anti inflammatory medications may reduce pain and inflammation, especially during flare ups. Your broader health history matters here, so medication should be used thoughtfully.
- Activity modification and ergonomic improvements can make a bigger difference than many people expect. Small changes in lifting, workstation setup, or sleep positioning can reduce daily strain.
- Epidural steroid injections may help when nerve inflammation is driving arm or leg symptoms. These are not a cure, but they can create a window for rehabilitation and return to movement.
- Weight management and exercise programs can reduce load on the spine and improve overall function. Even modest, sustainable changes can improve symptoms and endurance.
Surgical Care
Surgery is usually considered when conservative treatment is not effective, when pain becomes truly limiting, or when there is progressive weakness or significant nerve compression.
Depending on the diagnosis, surgical options may include decompression procedures to create more space for nerves, fusion surgery to stabilize painful or unstable segments, or disc replacement in select cases where motion preservation is appropriate.
The most important point is that spine surgery is not one size fits all. The right procedure depends on the condition, the specific anatomy involved, and the patient’s goals, including how they want to move and live in the years ahead.
Lifestyle Habits That Support a Healthy Spine After 50
If there is one message worth repeating, it is this: your spine responds to what you do consistently. The goal is to keep joints moving, muscles supportive, and bones strong.
- Low impact exercise is a strong starting point. Walking, swimming, and cycling help circulation, endurance, and joint health without excessive stress.
- Stretching supports flexibility, especially in the hips, hamstrings, and thoracic spine, which can reduce strain on the low back.
- Strength training helps preserve the muscle that protects your spine. This includes core work, glutes, and upper back strength to support posture.
- Nutrition matters more as you age. A balanced diet with adequate protein supports muscle, and calcium and vitamin D support bone health.
- Avoid tobacco and limit alcohol. Smoking is associated with poorer disc health and impaired healing, and heavy alcohol intake can affect balance and bone strength.
- Posture and ergonomics are not about sitting perfectly all day. They are about positioning your body so your spine is supported, your hips can move, and your muscles are not forced to compensate constantly.
When to See a Spine Specialist
Many people wait too long because they assume nothing can be done, or they worry that seeing a specialist automatically means surgery. In reality, a spine evaluation is often about clarity, reassurance, and a plan.
Consider an evaluation if you have:
- Pain that interferes with sleep, daily activities, or mobility
- Numbness, tingling, or weakness in the arms or legs
- Symptoms that persist despite home care
- Suspected osteoporosis or back pain after a fall
- Sudden loss of bladder or bowel control, which requires emergency care
The earlier you understand what is happening, the more options you typically have.
Why Choose Jeremy Smith, MD
Age related spine changes can be complex because they often involve multiple structures at once. Dr. Jeremy Smith is fellowship trained in complex spine surgery and has specific experience treating age related degeneration with both advanced non surgical strategies and modern surgical techniques when needed.
Patients appreciate an approach that focuses on function, comfort, and long term spine health. That means recommending the least invasive path that matches the problem, and building a treatment plan around the life you want to live, not just what shows up on imaging.
Schedule a Consultation
Age related spine changes do not have to limit your quality of life. If you are experiencing new back or neck symptoms after age 50, schedule a consultation with Dr. Jeremy Smith in Orange or Irvine to discuss your options and create a personalized plan to support a healthier, more active future.